Let’s start with the basics. Inside our lungs is a layer of mucus. Without this mucus, we could die. If the particles in the air we breathe were able to strike the lining of our lungs, we’d get so many infections that our immune systems wouldn’t be able to handle the workload.
Mucus doesn’t allow that to happen. It traps particles before they can attack our precious epithelial lung cells. Then tiny, hair-like filaments called cilia, which extend from the surface of epithelial cells, beat back and forth in a watery layer to move particle-laden mucus away from the cells and out of our lungs.
That’s the theory, anyway. But when UNC chemist Michael Rubinstein first heard it in 2001, he didn’t buy it. He couldn’t see how the cilia were able to stop mucus from penetrating the watery layer.
Ten years later, Rubinstein and UNC colleagues Brian Button, Richard Boucher, and Li-Heng Cai have discovered how those cilia really work. They describe their findings in the journal Science, upending the long-held theory while devising a new way to help patients with lung diseases.
Cilia are so tiny and thin that for a long time scientists struggled to get a good look at how they work and what’s going on around them. So back in 2001, researchers at UNCstarted the Virtual Lung Project. The idea was to gather researchers from different fields—applied math, chemistry, physics, medicine, computer science, biophysics, biochemistry—to discuss how to create a model, including visuals of cilia, that would help researchers solve health problems related to the lung. Rubinstein, who specialized in polymer theory and computer simulations, cofounded the project with lung researchers Richard Boucher and William Davis.
At the group’s first meeting, Davis and Boucher described the theory researchers around the world had accepted for decades: that the beating movement of cilia keeps mucus from expanding into the watery layer.
“I didn’t believe it,” Rubinstein says. “And it seemed as if they didn’t quite believe it, either.”
He offered an alternative. Maybe the cilia aren’t just whisper-thin projections. Rubenstein thought there might be something between the cilia that keeps the mucus from penetrating the watery layer.
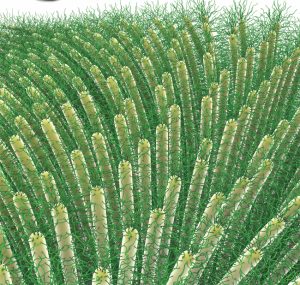
Here’s where things get a little complicated. What if the cilia had bristles like a hairbrush? What if these bristles, and not simply the beating of cilia, keep mucus out of the watery layer and provide cilia the opportunity to push mucus out of the lungs? If so, then researchers would have new information to use in their creation of treatments for lung diseases.
Rubinstein teamed up with Boucher, Button—a researcher atUNC’s cystic fibrosis center—and graduate student Li-Heng Cai to design experiments that could uncover what’s really going on in that layer of water where cilia beat.
In one experiment, the researchers froze a thin slice of the watery layer and used an electron microscope to zoom in between the cilia. What the researchers saw was an electron-dense, mesh-like structure. They weren’t sure what it was, but they suspected it was a mesh of mucins in between the cilia. They seemed to have found Rubinstein’s brush: mucins tethered to cilia.
Mucins are proteins found in gel-like secretions. For instance, the mucus layer above the cilia is a tangled mess of free-floating mucins and other molecules that bind to bacteria, viruses, and particles. But there are different kinds of mucins. Some, for example, aren’t sticky. And the mucins in the cilia mesh weren’t free-floating. They were attached to the cilia and formed a mesh, like a forest canopy.
Other researchers have found different kinds of mucins attached to cell membranes in human airways. Button’s team found that the mesh looks like those previously discovered mucins and macromolecules—essentially, sugars and proteins.
In another experiment, they removed mucus from cell cultures and added a solution full of particles of different types and sizes. They measured how far the particles penetrated the watery layer between cilia. The large particles couldn’t enter the watery layer. The medium-size particles could penetrate a little deeper. And the smallest particles could delve the deepest. This showed there was a mesh with larger gaps toward the top of the watery cilia layer and smaller gaps closer to the cell surface, Rubinstein says. It didn’t matter what kind of particle they used. All that mattered was the size and the fact that lung cells were protected from particles.
In describing their new model, the researchers say that mucins stick out of the cilia like bristles on a brush. The bristles are less dense at the top of a cilium and become denser toward the bottom, near the cell surface. This is why some particles can only delve so far into the mesh-like layer. Also, Rubinstein says, the bristles ensure that the cilia layer has a higher concentration of mucins than the mucus layer above it does. This also helps hold the mucus at bay. And it gave Rubinstein and Button’s team another idea when it comes to helping patients.
Rubinstein says that patients with lung problems have the same mesh-like structure and cilia function that healthy people have. The problem is that many respiratory ailments cause mucus to thicken. And as mucus thickens, its concentration of mucins increases. The mucus can then exert so much pressure that it sucks water from the cilia layer. “If the pressure is too high, then the mucus squashes the cilia,” Rubinstein says. This allows microorganisms to attack cell membranes and cause respiratory problems.
But Rubinstein and Button think that certain ailments, such as asthma, chronic obstructive pulmonary disease, and cystic fibrosis, have their own particular pressure ranges.
Based on their research, they’ve designed a method to measure the pressure of the mucus. “It’s like measuring blood pressure,” Rubinstein says. If the pressure is low, then the cilia brush can do its thing and the lungs function well. For instance, when cystic fibrosis patients get treatment, their mucus is made less thick and they can breathe better. But when the pressure climbs to a certain level, the cilia mesh can’t withstand the pressure. The cilia are crushed. The mucus isn’t cleared. And patients suffer the consequences.
Rubinstein and Button’s measurement method is helping them pinpoint an optimal pressure for mucus. As they perfect their method, they hope their measurements can give other researchers a clear target for developing strategies and therapies, such as drugs, that could help patients maintain proper mucus pressure in much the same way that doctors help people maintain optimal blood pressure.
Rubinstein and Button are now working to develop such strategies.
“In fact,” Rubinstein says, “I have to go to a meeting about that right now.”